
Intensive Care Unit (ICU): Inside the Critical Care Environment
The Intensive Care Unit (ICU), also known as the Critical Care Unit (CCU), is a specialized department within a hospital that provides comprehensive care for patients with life-threatening illnesses or injuries. It's a highly specialized environment equipped with advanced monitoring equipment and staffed by a dedicated team of healthcare professionals trained to manage complex medical conditions. This article delves into the intricacies of the ICU, exploring its purpose, infrastructure, patient population, monitoring techniques, common procedures, ethical considerations, and the vital role it plays in modern healthcare.
What is an ICU and Why is it Necessary?
The ICU serves as a crucial safety net for patients whose conditions require constant vigilance and immediate intervention. Unlike general hospital wards, the ICU provides a higher level of care due to:
- Continuous Monitoring: Patients are under constant observation, with vital signs (heart rate, blood pressure, respiration, oxygen saturation, etc.) continuously monitored and recorded. This allows for the rapid detection of subtle changes that could indicate a worsening condition.
- Advanced Life Support: The ICU is equipped to provide advanced life support measures, including mechanical ventilation, vasopressor support (medications to maintain blood pressure), dialysis, and other interventions necessary to sustain life.
- Specialized Staff: ICUs are staffed by highly trained physicians (intensivists), nurses, respiratory therapists, pharmacists, and other specialists who are experts in managing critically ill patients. The nurse-to-patient ratio is significantly lower in the ICU compared to general wards, allowing for more individualized attention.
- Rapid Response: The ICU team is prepared to respond immediately to medical emergencies, such as cardiac arrest or respiratory failure. This rapid response capability is critical for improving patient outcomes.
The necessity of the ICU stems from the fact that certain medical conditions can rapidly deteriorate, requiring immediate and intensive intervention. Conditions that commonly necessitate ICU admission include:
- Respiratory Failure: Patients who are unable to breathe adequately on their own, often requiring mechanical ventilation. This can be due to conditions like pneumonia, acute respiratory distress syndrome (ARDS), or chronic obstructive pulmonary disease (COPD) exacerbations.
- Cardiac Arrest: Patients who have experienced a sudden cessation of heart function. ICU care focuses on stabilizing the patient and addressing the underlying cause of the arrest.
- Severe Sepsis and Septic Shock: Patients with overwhelming infections that lead to organ dysfunction and dangerously low blood pressure.
- Major Trauma: Patients who have sustained significant injuries, such as those resulting from car accidents, falls, or violence.
- Post-Operative Care: Patients who have undergone complex surgeries that require close monitoring and support during the recovery period. This is particularly common after cardiac surgery, neurosurgery, or organ transplantation.
- Neurological Emergencies: Patients with conditions like stroke, traumatic brain injury, or seizures.
- Overdoses and Poisonings: Patients who have ingested toxic substances and require life support and detoxification.
- Severe Metabolic Disturbances: Patients with conditions like diabetic ketoacidosis (DKA) or severe electrolyte imbalances.
The ICU Environment: Design and Technology
The physical design and technological infrastructure of the ICU are meticulously planned to optimize patient care and safety. Key features of the ICU environment include:
Patient Rooms:
- Individual Rooms or Bays: ICUs may have individual rooms for each patient or open bays with multiple patients in a single area. Individual rooms offer greater privacy and can help reduce the spread of infection, while open bays allow for easier observation of multiple patients by the nursing staff.
- Monitoring Equipment: Each patient bed is equipped with a comprehensive array of monitoring equipment, including electrocardiogram (ECG) monitors, blood pressure monitors, pulse oximeters, and capnographs (which measure carbon dioxide levels in exhaled breath).
- Infusion Pumps: Multiple infusion pumps are used to deliver medications, fluids, and nutrition intravenously. These pumps allow for precise control over the rate and volume of infusions.
- Mechanical Ventilators: Ventilators provide respiratory support for patients who are unable to breathe adequately on their own. These machines deliver oxygen and control the rate and depth of each breath.
- Crash Cart: A crash cart containing emergency medications and equipment (e.g., defibrillator, intubation supplies) is readily available for immediate use in case of a medical emergency.
- Accessibility: Patient rooms are designed to allow for easy access by healthcare providers and equipment.
Central Monitoring Station:
A central monitoring station allows nurses to continuously monitor the vital signs of all patients in the ICU. Alarms are triggered when vital signs deviate from pre-set parameters, alerting the nursing staff to potential problems.
Medication Room:
A dedicated medication room is used for the safe storage and preparation of medications. This room is typically locked and access is restricted to authorized personnel.
Clean and Dirty Utility Rooms:
Separate clean and dirty utility rooms are essential for maintaining a sterile environment. The clean utility room is used for storing sterile supplies, while the dirty utility room is used for disposing of contaminated materials.
Isolation Rooms:
Isolation rooms are used to prevent the spread of infection from patients with contagious diseases. These rooms have special ventilation systems and require healthcare providers to wear protective gear (e.g., gowns, gloves, masks) when entering.
Technology in the ICU:
- Electronic Medical Records (EMRs): EMRs allow for the efficient storage and retrieval of patient information. This improves communication among healthcare providers and helps to ensure that patients receive the best possible care.
- Telemetry Systems: Telemetry systems allow for continuous monitoring of a patient's heart rhythm and other vital signs, even when the patient is not directly connected to a bedside monitor.
- Point-of-Care Testing: Point-of-care testing devices allow for rapid analysis of blood samples at the bedside. This allows for faster diagnosis and treatment.
- Imaging Equipment: Portable X-ray machines and ultrasound machines are often used in the ICU to obtain images of the chest, abdomen, and other areas of the body.
- Data Analytics: ICUs are increasingly using data analytics to identify trends and patterns in patient data. This can help to improve patient outcomes and reduce costs.
The ICU Team: Roles and Responsibilities
The ICU is staffed by a multidisciplinary team of healthcare professionals, each with their own unique roles and responsibilities. Effective teamwork and communication are essential for providing optimal patient care.
Intensivist:
The intensivist is a physician who specializes in the care of critically ill patients. They are responsible for leading the ICU team, developing treatment plans, and making critical decisions regarding patient care. Intensivists often have board certifications in critical care medicine, pulmonary medicine, or other related specialties.
Registered Nurse (RN):
ICU nurses provide direct patient care, including monitoring vital signs, administering medications, performing procedures, and providing emotional support to patients and their families. ICU nurses typically have specialized training and experience in critical care nursing. The nurse-to-patient ratio in the ICU is typically 1:1 or 1:2, allowing for close monitoring and individualized care.
Respiratory Therapist (RT):
Respiratory therapists are responsible for managing patients' respiratory needs, including mechanical ventilation, oxygen therapy, and airway management. They work closely with the intensivist and nurses to optimize respiratory support.
Pharmacist:
The pharmacist plays a crucial role in medication management, ensuring that patients receive the correct medications at the correct doses. They also monitor for drug interactions and adverse effects. ICU pharmacists are often highly specialized and have expertise in critical care pharmacology.
Physician Assistant (PA) / Nurse Practitioner (NP):
PAs and NPs may work in the ICU under the supervision of an intensivist. They can perform many of the same tasks as physicians, including ordering tests, prescribing medications, and performing procedures. They often provide continuity of care and help to ensure that patients receive timely and appropriate treatment.
Dietitian:
The dietitian assesses patients' nutritional needs and develops individualized nutrition plans. Adequate nutrition is essential for supporting healing and recovery in critically ill patients. Dietitians work closely with the medical team to ensure that patients receive the appropriate nutrients through oral, enteral (tube feeding), or parenteral (intravenous) routes.
Physical Therapist (PT) / Occupational Therapist (OT):
Physical and occupational therapists help patients regain their strength and function after a critical illness. They provide exercises, mobility training, and other therapies to help patients return to their previous level of activity. Early mobilization is often encouraged in the ICU to prevent complications such as muscle weakness and pressure ulcers.
Social Worker:
The social worker provides emotional support to patients and their families. They also help families navigate the complex healthcare system and access resources such as financial assistance and counseling services. Social workers play a critical role in addressing the psychosocial needs of patients and families during a stressful time.
Chaplain:
The chaplain provides spiritual support to patients and their families, regardless of their religious beliefs. They can offer prayer, counseling, and other forms of spiritual care. The chaplain can be a valuable resource for patients and families who are struggling to cope with a critical illness.
Common Monitoring Techniques in the ICU
Continuous monitoring of vital signs and other parameters is a cornerstone of ICU care. This allows for the early detection of changes in a patient's condition and the prompt initiation of treatment. Common monitoring techniques used in the ICU include:
Electrocardiogram (ECG):
ECG monitoring continuously records the electrical activity of the heart. This allows for the detection of arrhythmias (irregular heartbeats), ischemia (lack of blood flow to the heart), and other cardiac abnormalities.
Blood Pressure Monitoring:
Blood pressure can be monitored non-invasively using a cuff that is placed around the arm or leg. Invasive blood pressure monitoring involves inserting a catheter into an artery, allowing for continuous and more accurate measurement of blood pressure. Invasive monitoring is typically used in patients with unstable blood pressure or those requiring frequent blood draws.
Pulse Oximetry:
Pulse oximetry measures the oxygen saturation of the blood using a sensor that is placed on a finger or toe. This provides a non-invasive estimate of the percentage of hemoglobin that is carrying oxygen. Low oxygen saturation can indicate respiratory problems or inadequate oxygen delivery to the tissues.
Capnography:
Capnography measures the level of carbon dioxide (CO2) in exhaled breath. This can provide valuable information about a patient's respiratory status, including ventilation, perfusion (blood flow), and metabolism. Capnography is particularly useful in patients who are mechanically ventilated.
Central Venous Pressure (CVP) Monitoring:
CVP monitoring involves inserting a catheter into a large vein (e.g., subclavian, jugular) and measuring the pressure in the right atrium of the heart. CVP provides information about a patient's fluid status and cardiac function. It is often used to guide fluid resuscitation in patients with shock or heart failure.
Pulmonary Artery Catheter (Swan-Ganz Catheter) Monitoring:
A pulmonary artery catheter is inserted into a pulmonary artery and allows for measurement of pulmonary artery pressure, pulmonary capillary wedge pressure, and cardiac output. This provides more detailed information about cardiac function and fluid status than CVP monitoring. Pulmonary artery catheters are typically used in patients with complex cardiovascular problems.
Intracranial Pressure (ICP) Monitoring:
ICP monitoring involves inserting a sensor into the skull to measure the pressure inside the brain. This is used in patients with traumatic brain injury, stroke, or other conditions that can cause increased ICP. Elevated ICP can lead to brain damage and death.
Continuous Glucose Monitoring (CGM):
CGM systems continuously monitor blood glucose levels using a sensor that is inserted under the skin. This can help to improve glycemic control in patients with diabetes. Tight glycemic control is important in critically ill patients to reduce the risk of complications such as infection and organ dysfunction.
Neurological Monitoring:
Neurological monitoring can include assessment of level of consciousness, pupillary response, motor function, and sensory function. Electroencephalography (EEG) may be used to monitor brain activity in patients with seizures or other neurological disorders. Transcranial Doppler (TCD) ultrasound can be used to assess blood flow in the brain.
Common Procedures Performed in the ICU
In addition to monitoring, the ICU is equipped to perform a wide range of procedures to diagnose and treat critically ill patients. These procedures are often performed by intensivists, nurses, or other specialists.
Intubation and Mechanical Ventilation:
Intubation involves inserting a tube into the trachea (windpipe) to provide an airway. Mechanical ventilation uses a machine to deliver oxygen and assist with breathing. Intubation and mechanical ventilation are often necessary for patients with respiratory failure, altered mental status, or other conditions that compromise their ability to breathe adequately.
Central Line Placement:
Central line placement involves inserting a catheter into a large vein (e.g., subclavian, jugular, femoral) to administer medications, fluids, and nutrition. Central lines are also used to monitor CVP and draw blood samples.
Arterial Line Placement:
Arterial line placement involves inserting a catheter into an artery (e.g., radial, femoral) to continuously monitor blood pressure and draw blood samples for arterial blood gas (ABG) analysis. ABGs provide information about oxygenation, ventilation, and acid-base balance.
Lumbar Puncture:
A lumbar puncture involves inserting a needle into the spinal canal to collect cerebrospinal fluid (CSF). CSF is analyzed to diagnose infections, inflammation, and other neurological disorders.
Thoracentesis:
Thoracentesis involves inserting a needle into the pleural space (the space between the lung and the chest wall) to drain fluid. This may be necessary to relieve pressure on the lung or to diagnose the cause of a pleural effusion (fluid buildup in the pleural space).
Paracentesis:
Paracentesis involves inserting a needle into the abdominal cavity to drain fluid. This may be necessary to relieve pressure on the abdomen or to diagnose the cause of ascites (fluid buildup in the abdominal cavity).
Bronchoscopy:
Bronchoscopy involves inserting a flexible tube with a camera into the airways to visualize the trachea and bronchi. This can be used to diagnose lung diseases, remove foreign objects, or collect tissue samples for biopsy.
Placement of Feeding Tubes:
Feeding tubes are used to provide nutrition to patients who are unable to eat or swallow adequately. Nasogastric (NG) tubes are inserted through the nose into the stomach. Gastrostomy tubes (G-tubes) are surgically placed into the stomach through the abdominal wall. Jejunostomy tubes (J-tubes) are surgically placed into the jejunum (small intestine) through the abdominal wall.
Cardioversion and Defibrillation:
Cardioversion and defibrillation are procedures used to treat arrhythmias (irregular heartbeats). Cardioversion uses a controlled electrical shock to restore a normal heart rhythm. Defibrillation uses a high-energy electrical shock to stop a life-threatening arrhythmia such as ventricular fibrillation.
Dialysis:
Dialysis is a procedure that removes waste products and excess fluid from the blood when the kidneys are unable to function properly. Hemodialysis uses a machine to filter the blood. Peritoneal dialysis uses the lining of the abdomen to filter the blood.
Ethical Considerations in the ICU
The ICU is a setting where complex ethical dilemmas frequently arise. These dilemmas often involve decisions about life-sustaining treatment, end-of-life care, and patient autonomy. Ethical principles such as beneficence (acting in the patient's best interest), non-maleficence (avoiding harm), autonomy (respecting the patient's right to make decisions), and justice (fair allocation of resources) guide ethical decision-making in the ICU.
Informed Consent:
Informed consent is the process of obtaining a patient's permission to undergo a medical procedure or treatment after providing them with information about the risks, benefits, and alternatives. In the ICU, patients may be unable to provide informed consent due to their medical condition. In these cases, consent is typically obtained from a surrogate decision-maker, such as a family member or legal guardian.
Advance Directives:
Advance directives are legal documents that allow patients to express their wishes regarding medical treatment in the event that they are unable to make decisions for themselves. Advance directives can include a living will, which specifies the types of medical treatment that a patient would want or not want, and a durable power of attorney for healthcare, which designates a person to make healthcare decisions on the patient's behalf. It's crucial to have these documents available and followed in the ICU setting.
Withholding and Withdrawing Life-Sustaining Treatment:
Decisions about withholding or withdrawing life-sustaining treatment are among the most challenging ethical dilemmas faced in the ICU. These decisions should be made in consultation with the patient (if possible), the patient's family, and the healthcare team. Factors to consider include the patient's prognosis, quality of life, and wishes. Withholding treatment refers to not starting a new treatment, while withdrawing treatment refers to stopping a treatment that has already been started.
End-of-Life Care:
End-of-life care focuses on providing comfort and support to patients who are dying. This can include pain management, symptom control, and emotional and spiritual support. The goal of end-of-life care is to improve the patient's quality of life in their final days or hours. Hospice care is a specialized type of end-of-life care that is provided to patients who are expected to live for six months or less.
Resource Allocation:
Resource allocation refers to the distribution of limited healthcare resources, such as ICU beds, ventilators, and medications. In situations where resources are scarce, ethical principles such as justice and fairness must be considered when making decisions about who receives treatment. These are particularly sensitive topics and decisions during pandemics or other situations with strained resources.
Patient Privacy and Confidentiality:
Maintaining patient privacy and confidentiality is essential in the ICU. Healthcare providers must protect patients' personal information and medical records. Information about a patient's condition should only be shared with authorized individuals, such as family members or other healthcare providers who are involved in their care.
The Impact of ICU Stay on Patients and Families
An ICU stay can be a stressful and traumatic experience for both patients and their families. Patients may experience physical discomfort, pain, anxiety, and delirium. Families may feel overwhelmed, scared, and helpless. It's important to provide emotional support and information to both patients and families during this challenging time.
Delirium:
Delirium is a state of acute confusion that is common in ICU patients. It can manifest as disorientation, hallucinations, agitation, or lethargy. Delirium can have long-term consequences, including cognitive impairment and increased mortality. Strategies to prevent and manage delirium include minimizing sedation, promoting sleep, encouraging early mobilization, and providing cognitive stimulation.
Post-Intensive Care Syndrome (PICS):
PICS is a constellation of physical, cognitive, and psychological impairments that can persist after an ICU stay. Physical impairments can include muscle weakness, fatigue, and difficulty breathing. Cognitive impairments can include memory problems, difficulty concentrating, and impaired executive function. Psychological impairments can include anxiety, depression, and post-traumatic stress disorder (PTSD). Rehabilitation programs can help patients recover from PICS.
Family Support:
Families play a crucial role in supporting patients during and after an ICU stay. Healthcare providers should communicate regularly with families, provide them with updates on the patient's condition, and answer their questions. Families should be encouraged to visit the patient and participate in their care as much as possible. Support groups and counseling services can also be helpful for families who are struggling to cope with the stress of an ICU stay.
Communication:
Open and honest communication is essential for building trust between healthcare providers, patients, and families. Healthcare providers should explain the patient's condition and treatment plan in a clear and understandable manner. They should also listen to the patient's and family's concerns and address their questions. Regular family meetings can be helpful for discussing the patient's progress and making decisions about their care.
Bereavement Support:
If a patient dies in the ICU, it's important to provide bereavement support to the family. This can include offering condolences, providing information about grief and loss, and connecting them with resources such as grief counseling and support groups. Healthcare providers should also be sensitive to the family's cultural and religious beliefs.
The Future of ICU Care
The field of critical care medicine is constantly evolving, with new technologies and treatments being developed all the time. The future of ICU care is likely to be characterized by:
Personalized Medicine:
Personalized medicine involves tailoring treatment to the individual patient based on their genetic makeup, medical history, and other factors. This approach has the potential to improve patient outcomes and reduce the risk of adverse effects. In the ICU, personalized medicine could be used to optimize drug dosages, select the most appropriate ventilator settings, and predict which patients are at risk for complications.
Artificial Intelligence (AI) and Machine Learning (ML):
AI and ML are being used to develop new tools for monitoring, diagnosing, and treating critically ill patients. AI-powered algorithms can analyze large amounts of data to identify patterns and predict outcomes. For example, AI could be used to predict which patients are at risk for sepsis or to optimize ventilator settings in real time. The use of AI raises certain ethical considerations that must be addressed to protect patient data and privacy.
Telemedicine:
Telemedicine involves using technology to provide healthcare services remotely. Tele-ICUs can provide remote monitoring and support to hospitals that do not have 24/7 intensivist coverage. This can improve access to critical care services, particularly in rural areas.
Improved Monitoring Technologies:
New monitoring technologies are being developed to provide more detailed and accurate information about patients' physiological status. These technologies include wearable sensors, implantable devices, and advanced imaging techniques. These advances allow for earlier detection of problems and more timely intervention.
Focus on Prevention:
There is a growing emphasis on preventing critical illness in the first place. This includes strategies to reduce the risk of hospital-acquired infections, prevent falls, and manage chronic diseases. By preventing critical illness, we can reduce the need for ICU care and improve patient outcomes.
The Intensive Care Unit is a vital component of modern healthcare, providing life-saving care to patients with critical illnesses and injuries. Understanding the complexities of the ICU environment, the roles of the healthcare team, the monitoring techniques employed, the common procedures performed, and the ethical considerations involved is crucial for both healthcare professionals and the public. As technology advances and our understanding of critical illness grows, the ICU will continue to evolve, providing even more effective and personalized care to those who need it most.
Diğer Blog Yazıları
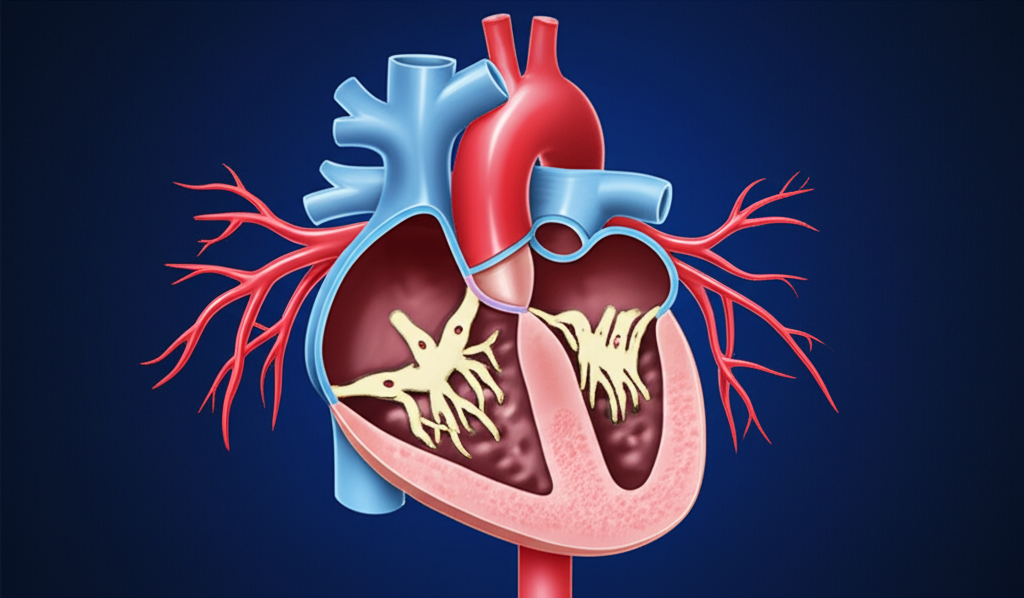
İnsan Kalbinin Anatomisi ve Kardiyovasküler Hastalıklarla İlişkisi
06 11 2025 Devamını oku »
İntensive Care Unit (ICU): Inside the Critical Care Environment
06 11 2025 Devamını oku »
Uyku Kalitenizi Artırmanın Bilimsel Yolları: Fizyolojik Temeller ve Pratik İpuçları
06 11 2025 Devamını oku »
Klinik Nörofizyoloji ile Tanısı Konulan Sık Görülen Hastalıklar
06 11 2025 Devamını oku »
Doğum Sonrası Yoğun Bakım: Annenin Sağlığı İçin Kritik Önlemler
06 11 2025 Devamını oku »
Akciğer Kanserinde Yeni Nesil Tedaviler: Hedefe Yönelik Terapiler ve İmmünoterapi
06 11 2025 Devamını oku »
Güneşin Zararlı Etkilerinden Korunma Yolları: Cildinizi Yaz Aylarında Nasıl Güvende Tutarsınız?
06 11 2025 Devamını oku »
Kronik Ağrıyla Yaşamak: Algoloji Uzmanlarından Destek Almanın Önemi
06 11 2025 Devamını oku »
Nükleer Tıp ile Kanser Teşhisinde Erken Tanının Önemi ve Güncel Uygulamalar
06 11 2025 Devamını oku »